Introduction: When the Liver Starts to Scar
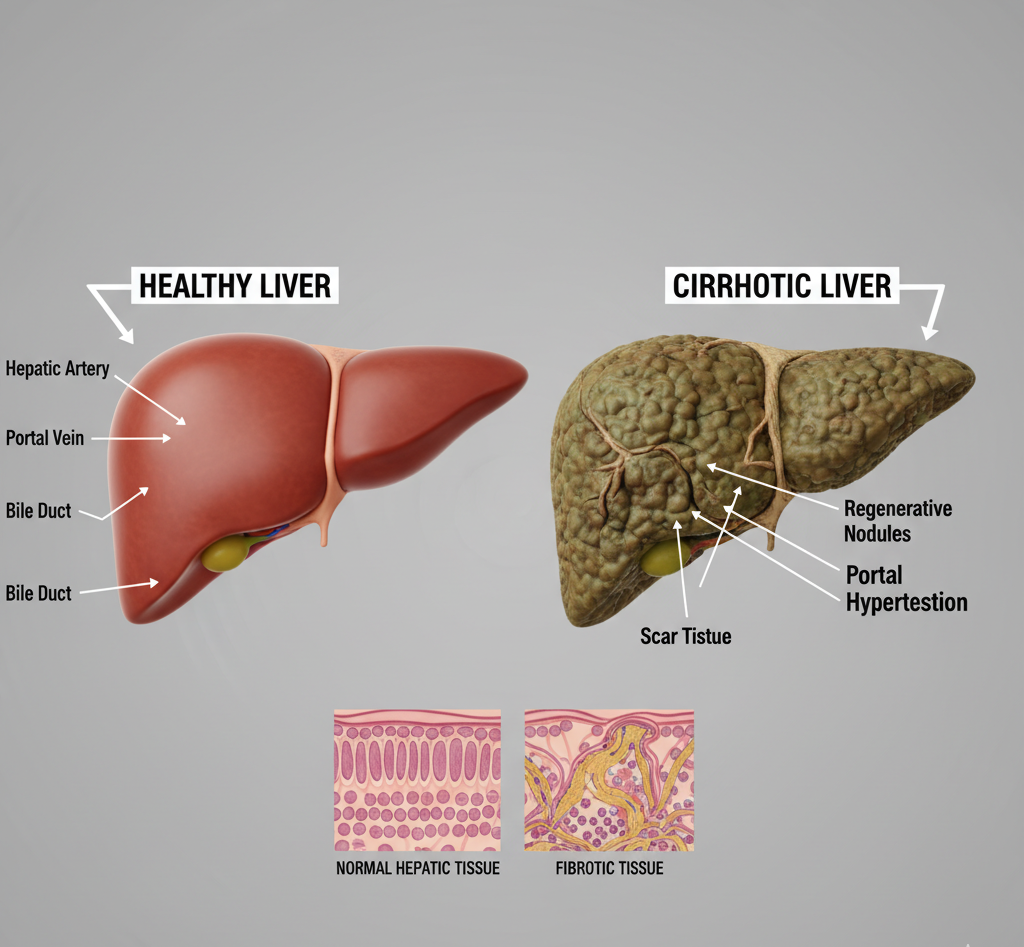
Your liver is one of the body’s most vital organs, responsible for detoxifying blood, storing nutrients, and aiding digestion. But when it becomes scarred from long-term damage, it leads to a serious condition called cirrhosis.
Cirrhosis happens when healthy liver tissue is replaced with scar tissue, preventing the organ from functioning properly. Over time, this damage is irreversible and can lead to liver failure.
In India, cirrhosis is one of the leading causes of death related to liver diseases — often linked to alcohol use, viral hepatitis, or fatty liver. Early diagnosis, lifestyle changes, and preventive healthcare can make a huge difference.
 What Is Cirrhosis?
What Is Cirrhosis?
Cirrhosis is the final stage of chronic liver disease. It develops gradually as continuous injury and inflammation cause fibrosis (scarring). The scarred tissue blocks blood flow through the liver, affecting its ability to detoxify the body.
As cirrhosis worsens, it can progress to end-stage liver failure — a life-threatening condition that may require a liver transplant.
Causes of Cirrhosis
Several factors can lead to cirrhosis:
-
Chronic alcohol abuse (Alcoholic liver disease)
-
Hepatitis B or C infection
-
Non-alcoholic fatty liver disease (NAFLD/NASH)
-
Autoimmune hepatitis
-
Genetic disorders (hemochromatosis, Wilson’s disease)
-
Prolonged use of certain medicines or toxins
Even repeated exposure to environmental chemicals or untreated liver infections can slowly damage the liver over years.
Symptoms of Cirrhosis
Early stages often show no symptoms, but as scarring progresses, you may experience:
-
Fatigue or weakness
-
Loss of appetite or weight loss
-
Yellowing of eyes and skin (jaundice)
-
Swelling in legs, feet, or abdomen (ascites)
-
Itchy skin
-
Easy bruising or bleeding
-
Spider-like blood vessels on the skin
-
Confusion or drowsiness (hepatic encephalopathy)
If you notice any of these symptoms, consult a hepatologist immediately.
Stages of Cirrhosis
-
Compensated Cirrhosis – Liver still functions, symptoms are mild or absent.
-
Decompensated Cirrhosis – Liver function declines; complications like jaundice, ascites, and bleeding occur.
Regular monitoring can help detect cirrhosis before it reaches the decompensated stage.
 Diagnosis of Cirrhosis
Diagnosis of Cirrhosis
Doctors diagnose cirrhosis through physical exams and specialized tests such as:
-
Liver Function Test (LFT) – Checks enzyme levels.
-
Ultrasound or FibroScan – Detects fibrosis and stiffness.
-
CT or MRI Scan – Detailed imaging of liver structure.
-
Liver Biopsy – Confirms scarring extent.
-
Blood Tests – To check for viral hepatitis and autoimmune causes.
Early detection is key to slowing disease progression.
Treatment for Cirrhosis
There is no complete cure for cirrhosis, but treatment can slow down or halt further damage.
1. Lifestyle and Diet Changes
-
Stop alcohol completely.
-
Eat a balanced, low-salt diet.
-
Maintain healthy weight and avoid fatty foods.
-
Stay hydrated and avoid processed foods.
2. Medications
-
Antiviral drugs for hepatitis.
-
Diuretics to reduce swelling.
-
Vitamin supplements (B-complex, A, D, E, K).
-
Lactulose to prevent confusion (hepatic encephalopathy).
3. Medical Procedures
-
Endoscopy for bleeding veins (varices).
-
Paracentesis for draining ascitic fluid.
-
Liver transplant in severe, end-stage cases.
Diet and Nutrition for Liver Health
A healthy diet plays a key role in managing cirrhosis.
Foods to include:
-
Fruits and vegetables (antioxidant-rich)
-
Whole grains and legumes
-
Lean protein (fish, eggs, tofu)
-
Olive oil and nuts in moderation
Foods to avoid:
-
Fried, oily, or spicy foods
-
Excess salt
-
Processed sugar and soft drinks
-
Alcohol in any form
Tip: Small, frequent meals help reduce pressure on the liver.
Complications of Cirrhosis
Untreated cirrhosis can lead to serious complications like:
-
Portal hypertension (high pressure in liver veins)
-
Variceal bleeding (internal bleeding in the esophagus)
-
Ascites (fluid buildup in abdomen)
-
Liver cancer
-
Kidney failure
-
Hepatic encephalopathy (confusion, coma)
When to See a Doctor
You should visit a liver specialist or gastroenterologist if you experience:
-
Persistent fatigue
-
Yellowing of eyes or skin
-
Swelling in legs or stomach
-
Unexplained weight loss or vomiting
Quickobook makes it easy to find verified hepatologists near you for timely evaluation and treatment.
Preventive Healthcare for Cirrhosis
-
Get vaccinated for hepatitis A and B.
-
Avoid alcohol and smoking.
-
Maintain a healthy weight.
-
Go for regular liver function tests.
-
Avoid unnecessary painkillers or herbal supplements.
-
Manage diabetes and cholesterol properly.
Remember: Prevention is the strongest protection for your liver.
Conclusion
Cirrhosis is a serious but manageable condition if detected early. A balanced lifestyle, regular check-ups, and preventive care can help protect your liver and prolong life.
If you have a history of alcohol use, hepatitis, or fatty liver, schedule a liver screening today. Early awareness saves lives — your liver deserves your care.
Quickobook CTA
Book a hepatologist or gastroenterologist on Quickobook for liver check-ups and cirrhosis management.
Visit Quickobook.com for easy doctor bookings, transparent fees, and reliable care.
Disclaimer:
This article is for educational purposes only. It is not a substitute for medical consultation or treatment. Always follow your doctor’s advice regarding diagnosis and care.
50 FAQs: Cirrhosis
Q1. What is cirrhosis?
A chronic liver disease where healthy tissue is replaced with scar tissue, reducing liver function.
Q2. Can cirrhosis be reversed?
Early stages may be controlled, but advanced scarring is permanent.
Q3. What causes cirrhosis?
Alcohol, hepatitis infections, fatty liver, and autoimmune conditions.
Q4. Is cirrhosis the same as liver failure?
No, but untreated cirrhosis can lead to liver failure.
Q5. Can you live long with cirrhosis?
Yes, with early diagnosis and proper care.
Q6. Does cirrhosis cause pain?
Some people feel discomfort or fullness in the right abdomen.
Q7. Can fatty liver turn into cirrhosis?
Yes, if inflammation and fat buildup continue for years.
Q8. Can cirrhosis be cured without transplant?
Treatment can slow damage but cannot reverse scarring.
Q9. How is cirrhosis diagnosed?
Through blood tests, ultrasound, and sometimes biopsy.
Q10. Is cirrhosis hereditary?
Some genetic disorders may cause it.
Q11. Can alcohol abstinence help?
Yes, quitting alcohol can stop further damage.
Q12. What are early warning signs?
Fatigue, poor appetite, and mild swelling.
Q13. Can hepatitis cause cirrhosis?
Yes, long-term Hepatitis B or C infections are major causes.
Q14. Can diet help reverse cirrhosis?
It supports recovery but cannot reverse advanced fibrosis.
Q15. What is portal hypertension?
Increased pressure in liver veins due to scarring.
Q16. Can cirrhosis cause itching?
Yes, due to bile salt accumulation.
Q17. Can it cause confusion?
Yes, toxins affect brain function (hepatic encephalopathy).
Q18. How is ascites treated?
Through diuretics or draining excess fluid.
Q19. Is liver transplant the only cure?
Yes, for end-stage or decompensated cirrhosis.
Q20. How can I protect my liver?
Avoid alcohol, eat healthy, and get vaccinated.
Q21. Can cirrhosis patients eat eggs?
Yes, in moderation for protein intake.
Q22. Can exercise help liver health?
Yes, regular light exercise improves metabolism.
Q23. What foods are good for liver health?
Leafy greens, fruits, fish, and olive oil.
Q24. Is cirrhosis contagious?
No, but hepatitis viruses that cause it can spread.
Q25. Can stress affect liver function?
Yes, chronic stress may worsen symptoms.
Q26. What is a FibroScan?
A non-invasive test to check liver stiffness.
Q27. Can cirrhosis cause vomiting blood?
Yes, due to variceal bleeding.
Q28. How much alcohol causes cirrhosis?
Varies — prolonged heavy drinking is the main factor.
Q29. Is coffee good for the liver?
Yes, it may lower the risk of fibrosis.
Q30. Can cirrhosis cause dark urine?
Yes, due to bilirubin buildup.
Q31. Can cirrhosis cause leg swelling?
Yes, due to poor circulation and protein loss.
Q32. Is jaundice common in cirrhosis?
Yes, it’s a typical symptom in later stages.
Q33. Can cirrhosis lead to cancer?
Yes, it increases the risk of liver cancer.
Q34. Can yoga help liver health?
Yes, gentle yoga improves circulation and stress levels.
Q35. Can cirrhosis patients fast?
Consult your doctor — it depends on your condition.
Q36. What is liver fibrosis?
Early scarring before full cirrhosis develops.
Q37. Can dehydration harm the liver?
Yes, it worsens toxin buildup.
Q38. How often should liver tests be done?
Every 6 months if you have risk factors.
Q39. Can cirrhosis cause fatigue?
Yes, it’s one of the most common symptoms.
Q40. Can milk thistle help?
It may support liver function under medical guidance.
Q41. Can cirrhosis affect sleep?
Yes, due to toxin buildup and fatigue.
Q42. Can children get cirrhosis?
Yes, due to genetic or biliary disorders.
Q43. How is liver transplant done?
The damaged liver is replaced with a healthy donor organ.
Q44. What are post-transplant precautions?
Regular follow-ups and immune-suppressing medicines.
Q45. Can I live a normal life with cirrhosis?
Yes, if managed properly and monitored regularly.
Q46. What is ascites in cirrhosis?
Fluid buildup in the abdomen due to poor liver function.
Q47. Can cirrhosis affect appetite?
Yes, it reduces digestion and hunger.
Q48. Can it cause depression?
Yes, due to chronic illness and fatigue.
Q49. How much does a liver test cost in India?
Around ₹800–₹3,000 depending on the test.
Q50. Where can I book a liver check-up?
Visit Quickobook.com to book liver tests or hepatologist appointments.









Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment