Introduction: The Alarming Rhythm of Your Own Heart
Have you ever been startled by a sudden, intense thumping in your chest? Perhaps a sensation of your heart momentarily stopping, only to restart with a forceful thump? These unnerving feelings are known as heart palpitations. They are one of the most common reasons people seek medical attention, yet they are also among the most confusing symptoms.
In a world where heart health is a major concern, recognizing the difference between a harmless flutter and a warning sign is crucial. The good news is that for the vast majority of people, palpitations are benign—a simple, albeit startling, reaction to stress, diet, or lifestyle. However, they can also be the first noticeable sign of an underlying cardiac condition, an arrhythmia (abnormal heart rhythm), that requires medical intervention. Knowing when to consult a specialist and how to book test efficiently can make all the difference.
This comprehensive 1500-word guide is designed to be your definitive resource. We will delve deeply into the common and rare causes, the diagnostic tools your doctor uses, the non-invasive management strategies you can adopt today, and the advanced medical treatments available for persistent or dangerous conditions. Our goal is to empower you with the knowledge to understand your body’s rhythm and take proactive steps toward optimal heart health.
Section I: Defining the Sensation – What Exactly is a Palpitation?
Heart palpitations are an abnormal awareness of your own heartbeat. Typically, we don't notice the 100,000 beats our heart makes each day. A palpitation happens when this silent, automated process becomes noticeable.
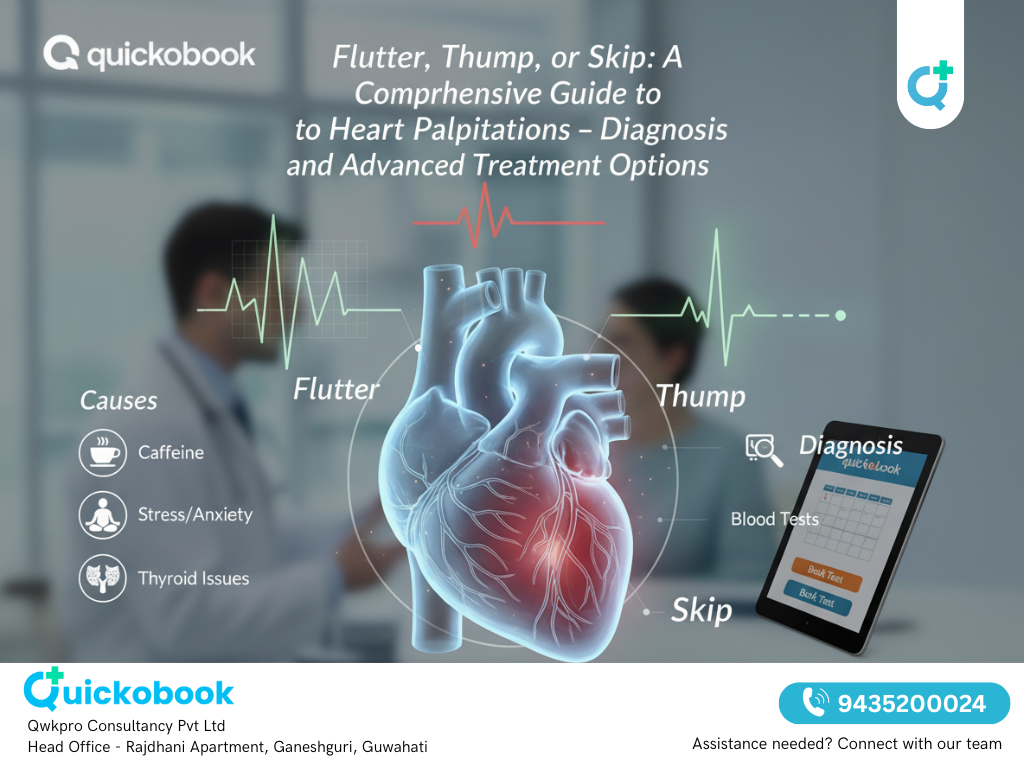
The sensation can manifest in several distinct ways, often described as:
- A Racing or Pounding Heart (Tachycardia): A feeling that your heart is beating extremely fast, often over 100 beats per minute.
- A Fluttering or "Flip-flopping": A rapid, often irregular, movement in the chest or throat.
- A Skipped or Missed Beat: This is usually the sensation after a Premature Ventricular Contraction (PVC) or Premature Atrial Contraction (PAC), where the early beat leads to a compensatory pause, and the following beat feels extra forceful.
- A Hard Thumping: A deep, powerful beat felt forcefully in the chest.
While the symptoms can vary, the underlying mechanism is a temporary disruption to the heart’s electrical system, the sophisticated circuitry that coordinates every beat.
Section II: Pinpointing the Cause – Common and Serious Triggers
Identifying the root cause of palpitations is the most important step in their management. Causes can be broadly categorized into lifestyle triggers, systemic non-cardiac conditions, and primary heart conditions.
A. The Vicious Cycle of Lifestyle and Emotional Triggers
For most individuals, palpitations stem from factors related to daily life and the nervous system. These triggers often lead to a surge in adrenaline and cortisol (stress hormones), which directly stimulate the heart muscle.
- Stress and Anxiety: This is arguably the single most common cause. During periods of intense worry, fear, or a full-blown panic attack, the body enters a “fight-or-flight” mode. Adrenaline is released, causing the heart to speed up, a normal physiological response that, when felt intensely, is perceived as a palpitation.
- Dietary Stimulants:
- Caffeine: High intake from coffee, tea, energy drinks, or even certain foods can over-excite the nervous system and directly increase heart rate.
- Alcohol: Excessive consumption, particularly binge drinking, is a well-known trigger for arrhythmias, sometimes dubbed “Holiday Heart Syndrome.”
- Nicotine: A powerful stimulant in all forms (cigarettes, vaping), nicotine constricts blood vessels and raises heart rate and blood pressure.
- Lack of Sleep and Fatigue: Chronic exhaustion can throw the body’s regulatory systems out of balance, increasing sensitivity to other triggers.
- Certain Medications and Supplements: Over-the-counter cold and cough medications containing pseudoephedrine or phenylephrine (decongestants), some asthma inhalers, and even certain herbal supplements (e.g., ephedra, ginseng) can directly act as stimulants.
B. Systemic (Non-Cardiac) Health Conditions
Sometimes, palpitations are a secondary symptom of a different health problem. Treating the root issue is the cure.
- Thyroid Imbalance (Hyperthyroidism): An overactive thyroid gland produces too much thyroid hormone (thyroxine). This hormone acts like a systemic accelerator, driving up metabolism and heart rate significantly.
- Anemia and Dehydration:
- Anemia: Low red blood cell count forces the heart to pump faster and harder to deliver sufficient oxygen to tissues, leading to noticeable pounding.
- Dehydration: Reduces blood volume, making the heart compensate by increasing its rate to maintain blood pressure.
- Electrolyte Imbalances: Key minerals like potassium, magnesium, and calcium are essential for the electrical conductivity of heart cells. Low or high levels can destabilize the heart’s rhythm.
- Hormonal Shifts: Palpitations are frequently reported by women during pregnancy, menstrual periods, and the peri-menopause/menopause transition due to fluctuating estrogen and progesterone levels.
C. Primary Cardiac Conditions (Arrhythmias)
When palpitations are frequent, severe, or occur with other serious symptoms, they may be caused by an underlying structural or electrical heart problem. Consulting a cardiologist is essential in these cases.
- Atrial Fibrillation (AFib): The most common type of serious arrhythmia. It involves a chaotic, rapid electrical activity in the upper chambers (atria), causing a fast and highly irregular heartbeat. AFib is a major risk factor for stroke.
- Supraventricular Tachycardia (SVT): Episodes of extremely fast heart rates that start in the upper part of the heart.
- Premature Contractions (PVCs/PACs): These are the "skipped beats." While usually harmless in a healthy heart, frequent PVCs can sometimes signal an underlying issue or weaken the heart muscle over time.
Section III: The Diagnostic Journey – Finding the True Rhythm
If you seek medical help for palpitations, your doctor will embark on a careful diagnostic process to rule out serious causes. The challenge in diagnosis is that the heart often returns to a normal rhythm by the time you reach the clinic. If your primary care physician suspects a heart issue, they will refer you to a cardiologist. You can use platforms like quickobook to easily book test appointments for the following procedures.
Key Diagnostic Tools:
- Electrocardiogram (ECG/EKG): A quick, non-invasive test that records the heart's electrical signals. A standard ECG can capture an arrhythmia if it is occurring at that moment, but its main use is to check for structural changes or scarring.
- Holter Monitor: Since palpitations are often transient, a portable ECG device is worn for 24 to 48 hours to continuously record heart activity during daily life. This helps the cardiologist connect symptoms to specific rhythm disturbances.
- Event Recorder/Mobile Cardiac Telemetry: If palpitations are infrequent, these small, wearable devices are used for up to 30 days or longer. They record data when the patient pushes a button after feeling a symptom or automatically capture significant rhythm disturbances.
- Blood Tests: Used to check for non-cardiac causes like thyroid hormone levels, electrolyte levels, and to screen for anemia. These can be arranged through your primary care provider or a cardiologist; remember to book test dates that work for you.
- Echocardiogram: An ultrasound of the heart that provides images of the heart's structure, valves, and pumping function, ruling out cardiomyopathy or valve disease.
- Stress Testing: Measures how the heart responds to physical exertion, often used to check for heart disease if symptoms occur mainly during activity.
Section IV: Treatment Strategies – From Lifestyle to Advanced Procedures
Treatment is always customized based on the confirmed cause. For the majority of cases, the solution lies in lifestyle adjustments.
READ ALSO: The Invisible Threat: High Blood Pressure, The Symptoms You Miss, And The Life-threatening Risks You Must Avoid
A. Non-Invasive Management and Lifestyle Hacks
For individuals whose palpitations are linked to stress, diet, or anxiety, these actionable steps can provide significant relief. These strategies are often recommended by your primary care doctor and cardiologist alike:
- Master Stress Reduction: Dedicate time daily to mental relaxation. Techniques like Mindfulness Meditation, Diaphragmatic Deep Breathing (slow, deep breaths), and Yoga can lower adrenaline levels and regulate the nervous system.
- Implement Vagal Manoeuvre’s: These tricks can sometimes immediately stop an episode of fast heartbeat (SVT):
- Valsalva Maneuver: Pinch your nose, close your mouth, and strain as if having a bowel movement for 10-15 seconds.
- Coughing: A strong, sustained cough.
- Cold Stimulus: Splashing ice-cold water on your face or applying an ice pack to the bridge of your nose.
- Hydration and Diet: Maintain optimal electrolyte balance by staying consistently hydrated and ensuring your diet includes mineral-rich foods (e.g., bananas, spinach, avocados for potassium and magnesium). Avoid large, heavy, or very sugary meals, which can sometimes trigger an episode.
- Quit Smoking and Limit Alcohol: These are non-negotiable for serious heart health. Develop a plan with your doctor to eliminate nicotine and moderate alcohol intake.
B. Pharmaceutical Interventions
If palpitations are caused by a diagnosed arrhythmia or a non-cardiac condition, medication is often the primary treatment strategy developed by your cardiologist.
- Beta-Blockers (e.g., Metoprolol, Atenolol): These are commonly prescribed to slow down the heart rate, block the effects of adrenaline, and reduce the frequency and intensity of palpitations.
- Calcium Channel Blockers (e.g., Diltiazem, Verapamil): These work by slowing the electrical signals traveling through the heart, primarily used to control fast heart rates in conditions like AFib.
- Antiarrhythmic Drugs: Medications like Amiodarone or Flecainide are used for more complex or persistent arrhythmias to help maintain a normal sinus rhythm.
- Blood Thinners (Anticoagulants): Essential for patients with AFib to prevent the formation of blood clots, thereby drastically reducing stroke risk.
C. Advanced Cardiology Procedures
For patients whose arrhythmias are life-threatening or unresponsive to medication, interventional procedures performed by a specialized cardiologist (an electrophysiologist) offer a curative or long-term management solution.
- Catheter Ablation: This is a highly effective, minimally invasive procedure. A specialist threads thin, flexible catheters through blood vessels to the heart. Once there, they identify the small areas of heart tissue that are causing the faulty electrical signals (the source of the arrhythmia). They then use radiofrequency (heat) or cryo (cold) energy to create tiny scars to ablate (destroy) this tissue, permanently blocking the irregular pathway and restoring a normal rhythm.
- Implantable Devices:
- Pacemaker: Used when the heart beats too slowly (bradycardia), a pacemaker sends small electrical pulses to keep the heart rate at a safe minimum.
- Implantable Cardioverter-Defibrillator (ICD): For patients at risk of sudden cardiac arrest (e.g., Ventricular Fibrillation), the ICD constantly monitors the heart and can deliver a life-saving electrical shock to reset the rhythm if a dangerously fast, chaotic beat is detected.
- Cardioversion: A procedure where a controlled electrical shock is delivered to the heart to instantly reset it back to a normal rhythm (sinus rhythm). It is typically used for conditions like AFib that have recently started or have persisted despite medication.
Conclusion: A Proactive Approach to Your Heart’s Rhythm
Heart palpitations are a powerful reminder that our cardiovascular system is always working. While they often resolve on their own, a proactive and informed approach is your best defense against both the anxiety they cause and the potential for a serious underlying condition.
The most important takeaway is this: Listen to your heart, but talk to your doctor.
If you experience frequent, worsening, or concerning palpitations, don't delay. You may need to book test appointments quickly to get a clear diagnosis. Modern platforms like quickobook make it easy to find and schedule necessary procedures like an ECG, Holter monitor, or an initial consultation with a cardiologist.
If your palpitations are brief and clearly linked to a trigger (like your fourth cup of coffee), you can start with lifestyle adjustments. But if they are persistent, frequent, or accompanied by any of the warning signs—chest pain, fainting, or severe shortness of breath—seek medical evaluation promptly.
By collaborating with your healthcare team, leveraging the right diagnostic tools, and committing to heart-healthy lifestyle choices, you can effectively understand and manage your heart’s rhythm, ensuring a strong, steady beat for a long life ahead. Take control of your heart health today.








Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment