Introduction
The Human Papillomavirus (HPV) vaccine has long been hailed as a major medical breakthrough in preventing cervical cancer and other HPV-related diseases. Now, a new long-term study has reaffirmed its effectiveness — showing that the vaccine offers strong, lasting protection for more than 10–15 years after immunization.
This discovery reinforces global and Indian health guidelines recommending HPV vaccination for adolescent girls and young women to protect their sexual and reproductive health.
In this Quickobook special, expert gynaecologists discuss what this new research means, how the vaccine works, and why early immunization is one of the most effective cancer-prevention steps a woman can take
 .
.
1. What Is HPV and Why It Matters
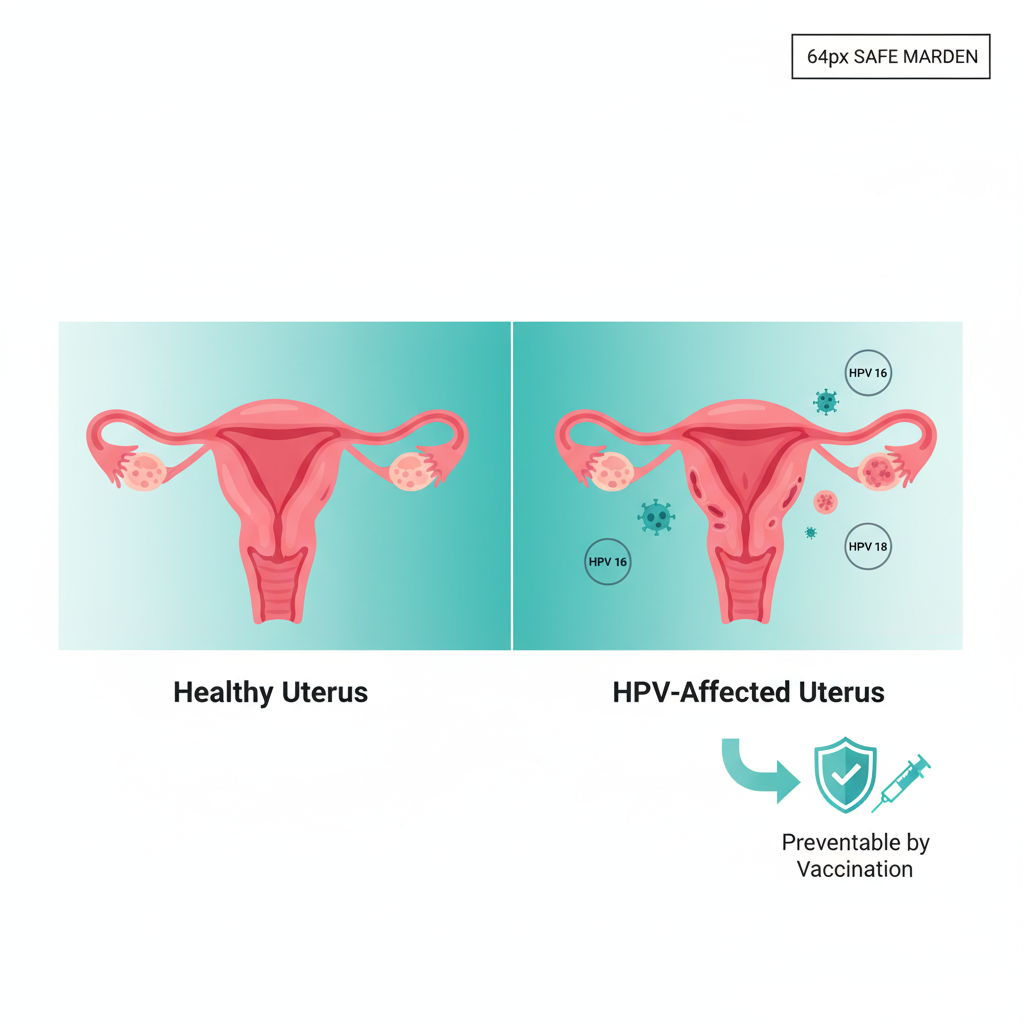
HPV (Human Papillomavirus) is one of the most common sexually transmitted infections (STIs) worldwide. More than 80% of sexually active people are exposed to HPV at some point in their lives.
While most infections clear on their own, certain high-risk HPV strains (especially types 16 and 18) can cause:
- Cervical cancer (the most common HPV-related cancer)
- Anal and vulvar cancers
- Oropharyngeal (throat) cancers
- Genital warts
Gynaecologist advice: HPV often causes no symptoms, making vaccination crucial before exposure. Preventing infection is far easier than treating cancer later.
2. The New Study: Long-Term Effectiveness Confirmed
The latest multinational study, published in The Lancet and supported by WHO, tracked over 25,000 vaccinated individuals for more than 15 years.
Key findings:
- The HPV vaccine maintained over 90% effectiveness in preventing infection with high-risk HPV strains.
- There was a 75–85% drop in cervical cancer precancerous lesions among vaccinated women.
- Protection remained strong even after a decade — with no need for booster doses in most cases.
This evidence proves that the vaccine provides long-lasting immunity and real-world protection against HPV-related cancers.

READ ALSO: Just 5 Extra Minutes Of Scrolling On The Toilet Can Raise The Risk Of This Disease By 46%, New Study Warns
3. How the HPV Vaccine Works
The HPV vaccine trains your immune system to recognize and fight HPV before it causes infection. It contains virus-like particles (VLPs) that mimic the virus structure but cannot cause disease.
When injected, your body produces antibodies that stay for years, protecting you if exposed later through sexual contact.
Types of HPV vaccines available in India:
- Cervarix: Protects against HPV 16 and 18
- Gardasil 4 / 9: Covers additional HPV types that cause warts and cancers
4. Who Should Get the HPV Vaccine?
The vaccine is most effective when given before the onset of sexual activity — ideally between ages 9–14. However, it can be administered up to age 45 based on doctor’s recommendation.
Recommended schedule:
- Ages 9–14: 2 doses, 6–12 months apart
- Ages 15–45: 3 doses over 6 months
Gynaecologist advice: Parents should include HPV vaccination as part of regular immunizations for girls — just like other preventive vaccines.
5. Why Early Vaccination Is Critical
Vaccinating before exposure ensures the body builds strong immunity against high-risk HPV strains before any infection can occur.
In India, where one woman dies of cervical cancer every 8 minutes, early protection can save thousands of lives.
HPV vaccination is now included in India’s National Immunization Programme (NIP) for girls aged 9–14, aiming to make cervical cancer a preventable disease.
6. Addressing Myths and Misconceptions
Despite proven safety, misinformation still prevents many from getting vaccinated. Let’s clear the air:
|
Myth |
Fact |
|
HPV vaccine causes infertility |
False. It has no effect on fertility or pregnancy. |
|
It’s only for women |
False. Boys can also benefit, preventing HPV spread and certain cancers. |
|
It’s unsafe |
False. WHO and DCGI confirm its excellent safety record. |
|
It promotes early sexual activity |
False. Studies show no link between vaccination and sexual behavior. |
Quickobook experts emphasize that HPV vaccination is about health and cancer prevention, not sexual behavior.
7. How the Vaccine Supports Sexual Health
HPV vaccination is part of a larger effort to promote safe and responsible sexual health.
Benefits include:
- Reduced transmission of sexually transmitted HPV types
- Lower risk of genital warts
- Better long-term reproductive health outcomes
- Empowerment through preventive care
Gynaecologist advice: Vaccination, regular Pap smears, and safe sexual practices together form a powerful defense against HPV-related disease.
8. Side Effects and Safety Profile
The HPV vaccine is among the safest vaccines ever studied. Reported side effects are usually mild and temporary, such as:
- Pain or swelling at injection site
- Mild fever or headache
- Dizziness or fatigue (short-term)
Severe reactions are extremely rare. Millions of doses have been safely administered globally.
9. HPV Vaccination in India: Current Scenario
India is gradually increasing HPV vaccine accessibility across states.
- Several states like Sikkim, Delhi, and Punjab have already introduced free vaccination programs for schoolgirls.
- The Indian government plans a nationwide rollout under the National Immunization Programme.
The cost of vaccination in private hospitals ranges from ₹2,000–₹3,000 per dose, but public programs aim to make it free for eligible age groups.
Quickobook helps you find trusted clinics and gynaecologists offering HPV vaccination and counseling near you.
10. Prevention Beyond Vaccination
While vaccination is the most powerful prevention tool, regular screening remains essential.
- Pap smear every 3 years for women aged 21–65
- HPV DNA test for early detection of viral presence
- Healthy habits: Avoid smoking, maintain hygiene, and limit multiple partners
Together, these steps can make cervical cancer a preventable and curable disease.
11. Global and Indian Success Stories
Countries like the UK, Australia, and Sweden have seen over 80% drop in cervical cancer rates after introducing nationwide HPV vaccination.
India is also moving forward — with growing awareness and support from the Ministry of Health and Family Welfare and public health platforms like Quickobook making vaccination information accessible to all.
12. Frequently Asked Questions (50)
Q1. What is the HPV vaccine for?
A1. It prevents infections from high-risk HPV strains that can cause cervical and other cancers.
Q2. When should girls take the HPV vaccine?
A2. Ideally between ages 9 and 14, before sexual activity begins.
Q3. Can boys take the HPV vaccine?
A3. Yes, it also protects boys against HPV-related cancers and warts.
Q4. Is the HPV vaccine safe?
A4. Yes, it has been proven safe through decades of global research.
Q5. How long does protection last?
A5. Studies show immunity lasting at least 15 years, likely lifelong.
Q6. Does the vaccine prevent all cervical cancers?
A6. It prevents about 90% of cases caused by HPV 16 and 18.
Q7. Are booster doses needed?
A7. Current data shows no booster is necessary.
Q8. Can vaccinated women skip Pap smears?
A8. No, regular screening is still important.
Q9. Does the vaccine help if I already have HPV?
A9. It won’t cure infection but can protect against other strains.
Q10. What are the side effects?
A10. Mild fever, pain, or redness at the injection site.
Q11. Is it covered under India’s immunization program?
A11. Yes, for girls aged 9–14 in select states, expanding nationwide soon.
Q12. Can pregnant women get vaccinated?
A12. It’s not recommended during pregnancy; postpone until after delivery.
Q13. Does the HPV vaccine protect against warts?
A13. Gardasil versions do; Cervarix does not.
Q14. What is the cost of HPV vaccination in India?
A14. Around ₹2,000–₹3,000 per dose in private clinics.
Q15. How many doses are needed?
A15. Two for girls under 15; three for older individuals.
Q16. Can men benefit from vaccination?
A16. Yes, it reduces throat and anal cancer risks.
Q17. Can HPV spread through non-sexual contact?
A17. Rarely; it spreads mainly through skin-to-skin sexual contact.
Q18. Why is early vaccination important?
A18. It ensures protection before any viral exposure.
Q19. Does India make its own HPV vaccine?
A19. Yes, Cervavac, India’s first indigenous HPV vaccine, launched recently.
Q20. Is Cervavac effective?
A20. Yes, it offers protection against major cancer-causing HPV strains.
Q21. Does HPV vaccine affect fertility?
A21. No, it has no impact on fertility.
Q22. Can HPV vaccine be given with other vaccines?
A22. Yes, it can be co-administered safely.
Q23. Can adults above 26 take the vaccine?
A23. Yes, up to age 45 after consulting a doctor.
Q24. Does the vaccine cure existing cancer?
A24. No, it’s preventive, not therapeutic.
Q25. What is the spacing between doses?
A25. Usually 6 months between the first and last dose.
Q26. Is the HPV vaccine mandatory?
A26. Not mandatory but strongly recommended.
Q27. Are there any cultural concerns in India?
A27. Awareness and education are improving acceptance.
Q28. What if I miss a dose?
A28. Resume as soon as possible; don’t restart the series.
Q29. Can the vaccine cause infection?
A29. No, it contains no live virus.
Q30. Is it painful?
A30. Mild injection pain only.
Q31. Is it safe for diabetic or hypertensive patients?
A31. Yes, but always inform your doctor.
Q32. How is HPV linked to cancer?
A32. Persistent infection causes abnormal cell changes that lead to cancer.
Q33. Can oral sex transmit HPV?
A33. Yes, it can spread to the mouth or throat.
Q34. What are the warning signs of cervical cancer?
A34. Irregular bleeding, pelvic pain, or foul discharge.
Q35. Can HPV infection go away on its own?
A35. Yes, most mild infections clear within 2 years.
Q36. Can I take the vaccine after HPV infection?
A36. Yes, for protection against other strains.
Q37. What lifestyle changes help prevent HPV?
A37. Safe sex, regular screening, and no tobacco use.
Q38. Can HPV affect pregnancy?
A38. Rarely; consult your gynaecologist if infected.
Q39. What is the difference between Cervarix and Gardasil?
A39. Cervarix covers 2 strains, Gardasil covers up to 9.
Q40. How soon after vaccination does protection start?
A40. Within a few weeks after the second dose.
Q41. Can vaccinated people still spread HPV?
A41. Very unlikely, as infection risk is drastically reduced.
Q42. Is HPV vaccination required for men in India?
A42. It’s optional but recommended for added protection.
Q43. Does insurance cover HPV vaccination?
A43. Some health plans and preventive care packages do.
Q44. How often should women get Pap smears?
A44. Every 3 years after age 21.
Q45. Can diet help prevent HPV infections?
A45. A healthy immune system helps fight infections better.
Q46. Is there a cure for HPV?
A46. No, but the body’s immune system clears most infections.
Q47. What is HPV DNA testing?
A47. A screening test that detects high-risk HPV strains early.
Q48. Can HPV affect men’s fertility?
A48. Rarely, but chronic infections may cause genital issues.
Q49. How can I find vaccination centers near me?
A49. Use Quickobook to locate authorized clinics and doctors.
Q50. Can HPV vaccination eliminate cervical cancer completely?
A50. Combined with screening, it can make cervical cancer nearly extinct.
Conclusion
The new study proves what doctors have long believed — the HPV vaccine provides long-term, powerful protection against cancer-causing viruses.
By getting vaccinated early, following regular screenings, and maintaining good sexual health habits, women can drastically lower their risk of cervical and related cancers.
Through Quickobook, you can easily connect with qualified gynaecologists, book vaccinations, and receive expert advice on HPV prevention and women’s health.
Quickobook CTA
Book your HPV vaccination appointment or consult a gynaecologist near you through Quickobook — India’s trusted platform for safe, affordable, and confidential healthcare.
Disclaimer
This article is for educational purposes only and not a substitute for professional medical advice. Always consult your gynaecologist before taking any vaccine or treatment.







Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment