Introduction
Long COVID has emerged as one of the most significant COVID complications in recent years, affecting millions of people worldwide—even long after the initial infection has resolved. While both men and women can develop long COVID, research consistently shows that women are more likely to experience persistent or severe long COVID symptoms, particularly those related to fatigue, brain fog, hormonal imbalance, autoimmune flare-ups, and mental health challenges.
In India as well, healthcare professionals have observed that women—especially between the ages of 20 and 50—show a higher tendency to develop sustained symptoms weeks or even months after recovering from the virus. This raises important questions: Why are women more at risk? What makes their experience different? How do biology, hormones, immunity, and lifestyle interact to create this vulnerability?
This comprehensive guide explains the science behind gender differences in long COVID, the most common symptoms in women, risk factors, diagnosis, treatments, lifestyle tips, and when to seek medical help. Written in simple, patient-friendly language, this blog is designed to help Indian women understand their bodies better and take informed steps toward recovery.
What Is Long COVID?
Long COVID refers to symptoms that continue for weeks or months after the initial COVID-19 infection has resolved. These symptoms can affect multiple organs and may appear even after a mild or asymptomatic infection.
Commonly used terms include:
-
Post-COVID syndrome
-
Post-acute COVID
-
Long-haul COVID
-
Post-COVID complications
According to recent reports, 10–30% of people infected with COVID-19 develop long COVID, but the percentage is significantly higher in women.
Why Women Are More Prone to Long COVID
Several factors—biological, hormonal, genetic, and social—combine to increase the risk of long COVID in women.
Here are the major reasons:
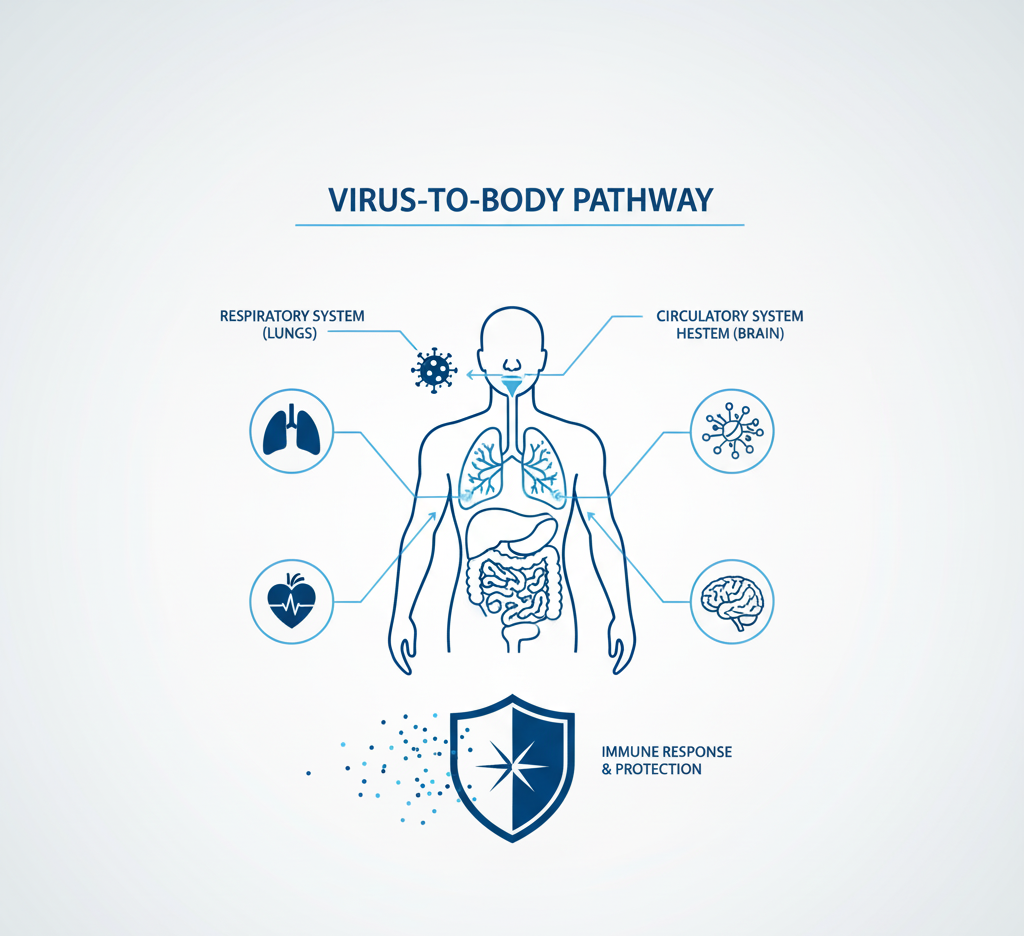
Stronger but More Reactive Immune Systems
Women naturally have a stronger immune system than men, which helps them fight viruses more effectively. However, this also increases the risk of an overactive immune response, which may contribute to long-lasting inflammation after COVID.
An overly active immune system may cause:
-
Fatigue
-
Muscle pain
-
Joint stiffness
-
Brain fog
-
Persistent inflammation affecting heart, lungs, and nerves
This immune “overdrive” is one of the leading explanations for the higher prevalence of long COVID in women.
Hormonal Influence, Especially Oestrogen
Hormones play a major role in modulating the immune system. Oestrogen, the dominant female hormone, boosts immunity and increases inflammatory responses. In long COVID, this heightened sensitivity can worsen symptoms.
Women may notice stronger symptoms:
-
Before periods
-
During perimenopause
-
During menopause
-
After pregnancy
-
During hormonal therapies
Fluctuating hormones can intensify long COVID symptoms like fatigue, mood swings, headaches, and joint pain.
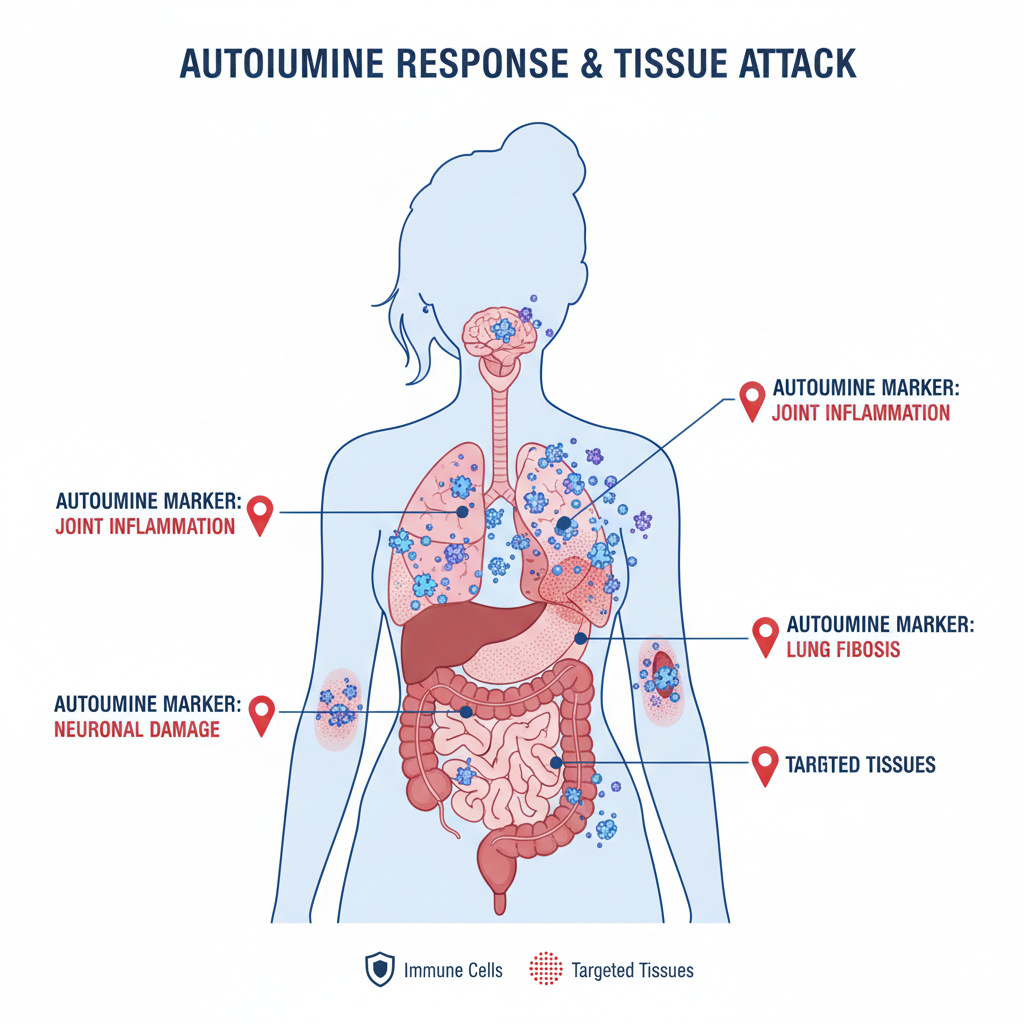
Autoimmune Predisposition
Women are far more likely than men to develop autoimmune diseases like:
-
Thyroid disorders
-
Lupus
-
Rheumatoid arthritis
-
Multiple sclerosis
Because long COVID behaves like an autoimmune condition in many patients, this predisposition makes women more vulnerable.
The virus may trigger:
-
Autoimmune flare-ups
-
New autoimmune reactions
-
Chronic inflammation
-
Muscle weakness
-
Heart palpitations
Higher Risk During Reproductive Years
Studies show that women aged 25–50 report the highest rates of long COVID. This age group experiences:
-
Active menstruation cycles
-
Pregnancy
-
Postpartum changes
-
Family and professional stress
These factors increase the chances of hormonal imbalance and immune fluctuation.
Impact of Stress and Mental Health
Women often face higher levels of chronic stress due to work, family responsibility, caregiving roles, and societal expectations. Stress weakens immunity and worsens long COVID symptoms such as:
-
Anxiety
-
Sleep problems
-
Brain fog
-
Fatigue
-
Depression
Cortisol imbalance may delay complete recovery.
Differences in Body Composition
Women usually have:
-
Higher body fat percentage
-
Different metabolic rates
-
Different fat distribution
These factors influence how the virus affects the body and how the immune system responds.
Body fat stores inflammatory molecules, which play a role in long COVID severity.
Social and Diagnostic Factors
Women’s symptoms are often underdiagnosed or dismissed as:
-
Anxiety
-
Hormonal issues
-
Stress
-
Psychosomatic symptoms
This can delay proper evaluation and treatment, causing symptoms to persist longer.
Common Long COVID Symptoms in Women
Women experience a wide range of symptoms, some more frequently than men.
Most common ones include:
-
Severe fatigue
-
Brain fog
-
Memory issues
-
Rapid heartbeat
-
Shortness of breath
-
Chest discomfort
-
Joint pain
-
Hair fall
-
Menstrual irregularities
-
Anxiety
-
Depression
-
Insomnia
-
Loss of smell or taste
-
Digestive problems
-
Low energy after minor tasks
-
Dizziness
Women with pre-existing conditions like PCOS, thyroid disorders, anaemia, or asthma may have more severe symptoms.
Menstrual and Reproductive Health Effects
Long COVID can affect the menstrual cycle and reproductive system.
Some reported issues include:
-
Delayed periods
-
Heavier periods
-
Irregular cycles
-
Increased cramps
-
Spotting
-
Lower fertility markers
-
Aggravation of PCOS
-
Worsened PMS
These symptoms often relate to inflammation and hormonal imbalance triggered by long COVID.
Heart and Circulation-Related Symptoms in Women
Women may be more prone to cardiovascular long COVID complications such as:
-
Palpitations
-
Chest tightness
-
POTS (Postural Orthostatic Tachycardia Syndrome)
-
Shortness of breath
-
Lightheadedness
These may worsen during periods or menopause.
Mental Health Impact on Women
Women report higher psychological distress during and after COVID.
Common experiences include:
-
Low mood
-
Constant worry
-
Sleep disturbance
-
Difficulty concentrating
-
Emotional sensitivity
Stress fuels inflammation, creating a cycle that delays recovery.
Diagnosis of Long COVID in Women
There is no single test for long COVID. Diagnosis is based on symptoms that persist beyond 4–12 weeks after infection.
Doctors may recommend:
-
Blood tests
-
Vitamin levels
-
Hormonal panel
-
Thyroid tests
-
Lung function tests
-
ECG or Holter
-
Echocardiography
-
Chest X-ray or CT scan
-
MRI brain if needed
-
Autoimmune screening
Tracking symptoms in a diary can help the doctor make a clearer diagnosis.
ALSO READ: Workplace Stress And Rising Diabetes Risk Among India’s Working-age Adults
Treatment for Long COVID in Women
Treatment focuses on managing symptoms and supporting recovery.
Common approaches include:
Medication Support
-
Anti-inflammatories
-
Supplements (vitamin D, vitamin B12, zinc)
-
Hormonal balancing if needed
-
Thyroid medication
-
Nebulisation
-
Allergy medications
-
Sleep support medicines if prescribed
Therapies
-
Breathing physiotherapy
-
Heart rehabilitation
-
Cognitive behavioural therapy
-
Mental health counselling
-
Pelvic floor therapy for reproductive concerns
-
Physical therapy for muscle weakness
Lifestyle Adjustments
-
Low-inflammatory diet
-
Adequate rest
-
Structured exercise
-
Stress management
-
Sleep hygiene
Treatment should always be customized.

Lifestyle Tips to Reduce Long COVID Symptoms
Balanced Diet
-
Fresh vegetables and fruits
-
High-quality protein
-
Hydrating foods
-
Healthy fats
-
Avoid sugary and processed foods
Breathing Exercises
-
Diaphragmatic breathing
-
Pursed-lip breathing
-
Anulom-vilom
-
Deep lung expansion techniques
Mind-Body Techniques
-
Yoga
-
Meditation
-
Journaling
-
Relaxation therapy
Physical Activity
-
Slow walking
-
Stretching
-
Light strengthening
-
Pacing strategies
-
Avoid pushing too hard
Sleep Routine
-
Reduce screen time
-
Fixed sleep schedule
-
Warm bath
-
Calm environment
When to See a Doctor
Seek medical help if symptoms worsen or persist beyond 4 weeks after COVID.
Urgent symptoms include:
-
Persistent high heart rate
-
Severe shortness of breath
-
Chest pain
-
Fainting
-
Extreme fatigue
-
Depression or anxiety
-
Irregular periods
-
Hair fall with scalp changes
-
Worsening headaches
-
Lightheadedness
-
Very low energy after simple tasks
Early treatment improves recovery.
Risks & Complications in Women
If ignored, long COVID may cause:
-
Chronic fatigue syndrome
-
Depression
-
Anxiety disorders
-
Heart rhythm issues
-
Autoimmune flare-ups
-
Hormonal imbalance
-
Fertility disruptions
-
Long-term lung changes
-
Persistent inflammation
-
Decreased quality of life
Long COVID can affect daily activities, work performance, emotional well-being, and family responsibilities.
50 FAQs on Women and Long COVID
-
Why are women more likely to get long COVID?
Because their immune systems are stronger and more reactive. -
Does long COVID affect women differently?
Yes, women often have more fatigue, hormone changes, and autoimmune symptoms. -
Can hormones make long COVID worse?
Yes, oestrogen fluctuations can intensify symptoms. -
Are women in their 20s–40s at higher risk?
Yes, due to active hormonal cycles. -
Do periods worsen long COVID symptoms?
Many women report increased fatigue and pain around menstruation. -
Can long COVID affect fertility?
It may temporarily affect menstrual cycles or ovulation. -
Does long COVID increase anxiety?
Yes, it often affects mental health. -
Is hair fall common in long COVID?
Very common in women. -
Can long COVID cause thyroid issues?
Yes, it may trigger thyroid imbalance. -
Do women get more autoimmune reactions post-COVID?
Yes, due to higher autoimmune predisposition. -
Can long COVID cause irregular periods?
Yes, many women experience cycle changes. -
Does stress worsen long COVID in women?
Yes, stress increases inflammation. -
Can long COVID cause chest pain?
Yes, but needs evaluation to rule out heart involvement. -
Is shortness of breath common?
Yes, especially in women with lung sensitivity. -
Can long COVID cause dizziness?
Yes, often due to POTS or blood pressure changes. -
Do women experience more fatigue than men?
Studies say yes. -
Is joint pain normal in long COVID?
Yes, inflammatory reactions can cause it. -
Can long COVID trigger migraines?
Yes, especially in women with prior migraine history. -
Are hormonal treatments helpful?
Some women improve, depending on the cause. -
Can long COVID cause brain fog?
Yes, widely reported. -
Is depression common in long COVID?
Yes, in both men and women but more in women. -
Does long COVID affect sleep?
Yes, insomnia is common. -
Can breathing exercises help?
Yes, they improve lung capacity. -
Should women with PCOS be more cautious?
Yes, they may experience worse symptoms. -
Does long COVID affect breastfeeding?
Usually safe, but fatigue may affect energy levels. -
Can long COVID worsen asthma?
Yes, especially in winter. -
Is weight gain common?
Yes, due to reduced activity and metabolism issues. -
Can long COVID affect digestion?
Yes, bloating, acidity, and IBS-like symptoms occur. -
Can long COVID cause palpitations?
Yes, especially in young women. -
Should women get checked for vitamin deficiencies?
Yes, especially vitamin D and B12. -
Does exercise help long COVID?
Yes, but start slow and increase gradually. -
Can long COVID mimic thyroid disease?
Yes, symptoms are similar. -
Is long COVID dangerous?
It can be serious if not managed. -
Can women with diabetes have worse long COVID?
Yes, due to inflammation. -
Is long COVID permanent?
Most people recover with time. -
Can long COVID affect skin?
Yes, rashes, dryness, and acne may occur. -
Can antidepressants help?
If prescribed, they may help manage mood symptoms. -
Is long COVID linked to menopause?
Symptoms may overlap with menopausal symptoms. -
Do women need lung tests for long COVID?
If breathlessness persists, yes. -
Can long COVID affect blood pressure?
Yes, fluctuations are common. -
Is chest tightness normal?
Yes, but it requires evaluation. -
Can long COVID cause memory issues?
Yes, memory lapses and concentration problems occur. -
Is yoga helpful?
Yes, it reduces stress and inflammation. -
Should women take multivitamins?
If recommended by a doctor. -
Can long COVID cause extreme tiredness?
Yes, chronic fatigue syndrome may develop. -
Do long COVID symptoms come and go?
Yes, flare-ups are common. -
Can long COVID cause allergies?
Yes, increased sensitivity is reported. -
Are home remedies helpful?
Some help with mild symptoms. -
Can long COVID affect work performance?
Yes, due to fatigue and brain fog. -
How long does long COVID last?
It varies—weeks to months, depending on severity.
Conclusion
Women around the world are disproportionately affected by long COVID due to biological, hormonal, immune, and social factors. Early recognition and timely care can significantly improve outcomes. Whether it’s fatigue, breathlessness, hormonal imbalance, or emotional stress, long COVID needs a supportive and personalised approach.
Women must prioritise self-care, get adequate rest, maintain a healthy lifestyle, and consult a doctor if symptoms persist.
Quickobook CTA
If you’re experiencing post-COVID symptoms, book a consultation with a General Physician, Pulmonologist, Cardiologist, or Gynaecologist on Quickobook.
Fast appointments. Verified doctors. Easy follow-ups.
Disclaimer:
This blog is for educational purposes only and should not replace medical consultation. Always speak with a qualified doctor for personalised diagnosis and treatment.










Comments (0)
No comments yet. Be the first to share your thoughts!
Leave a Comment